Conflict in Nigeria: Why Access to Health Care is a Luxury Few Can Afford

For Australians, it might be difficult to imagine a scenario where there are no hospitals to walk into or no medical personnel to consult about the most basic of health issues. But this is the reality for thousands of people affected by the ongoing armed conflict in northeastern Nigeria.
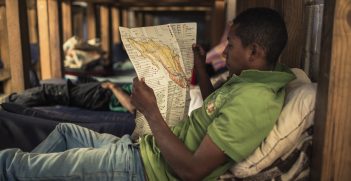
The conflict, which began in 2009 in the state of Borno, escalated rapidly, engulfing the neighboring states of Adamawa and Yobe before fanning out to the neighboring countries of Chad, Niger and Cameroon. Ten years on, the armed conflict has displaced more than two million people, with those who attempt to return home often forced to leave again. The situation has generated massive humanitarian needs: for sources of sustained livelihood, shelter, food, clean water, sanitary materials and space, as well as the need to find missing family members. However, one of the most pressing needs in this area has always been access to health care systems and personnel.
Nigeria’s northern region has historically been beset by skewed development in terms of social, educational, economic and health care systems. The region has been the focus of much data-driven discussion regarding issues like the education of young girls, child and maternal mortality rates and access to health care. Before the outbreak of the conflict, access to health care systems was considerably poorer compared to other parts of the country. Often, women and children are the ones who bear the harshest consequences of a flailing health care system.
Since 2012, The International Committee of the Red Cross (ICRC) has worked in the northeastern states affected by the conflict to ensure that access to health care is a priority for affected populations. From setting up mobile surgical teams to supporting 20 primary health care centers across the region, the ICRC constantly seeks ways to ensure affected populations access health care in a dignified, safe and professional manner. In 2018 alone, over 500,000 consultations were made across the ICRC-supported health care centers while more than 10,000 children under the age of five suffering from severe acute malnutrition were treated. In areas where security remains highly volatile, the ICRC trained and equipped traditional birth attendants. Over 22,900 children have been birthed across the 20 clinics supported by the ICRC or at home with these trained traditional birth attendants.
Great strides are being made in the effort to improve health care access, yet needs on the ground continue to outnumber the strength of current interventions. This gap is made even wider by the constant threat to security and access for humanitarian workers in the region. The humanitarian community suffered a severe tragedy last year when one nurse and two midwives were taken hostage by a non-state armed group. The midwives who were working in an ICRC-supported health facility in Rann at the time were eventually killed while the nurse, a UN staffer, remains in captivity. Rann, a town located in the Kala Balge local government of Borno state, had already been the focus of attention before the attacks and continues to feature in the news. In January this year, intensified attacks in the area led to massive displacements of more than 30,000 persons to Cameroon. An ICRC health facility was burned down in the process and humanitarian assistance materials destroyed.
The recent return of these displaced people back to their homes in Rann underlines the need for guaranteed access and safety for humanitarian workers to strengthen their interventions. These returnees have come back to a place where the health care systems are in a fragile state with limited options of functioning health care facilities and very few numbers of medical personnel willing to work in an area known for its volatility.
Alhaji Bukar Sanda, a medical doctor who works as a health field officer for the ICRC in Borno paints a rather bleak picture about the options the returning population will have. He describes how anyone needing medical attention in Rann will have to be transported by a cart-pulling donkey because of the restriction on vehicle movement in the area. While the nearest health facility is in Ngala, some 30 kilometres away, due to the insecurity the residents prefer to go to the General Hospital in Mada, some 37 kilometres on the border town of Cameroon, even if several security check-points on the way make the journey longer.
“No one should go through so much trouble to see a doctor”, Doctor Bukar says.
He also explains that medical personnel prefer to stay in Maiduguri metropolis, for safety reasons, whereas greater needs exist in the outskirt villages.
Access to basic health care should be a given for all people, but the armed conflict in northeast Nigeria has made being healthy a luxury that affected communities simply cannot afford.
Eleojo Esther Akpa is an editor and analyst for the International Committee of the Red Cross, Nigeria.
This article is published under a Creative Commons Licence and may be republished with attribution.